New test could save lives from deadly fungal infection which spiked during pandemic
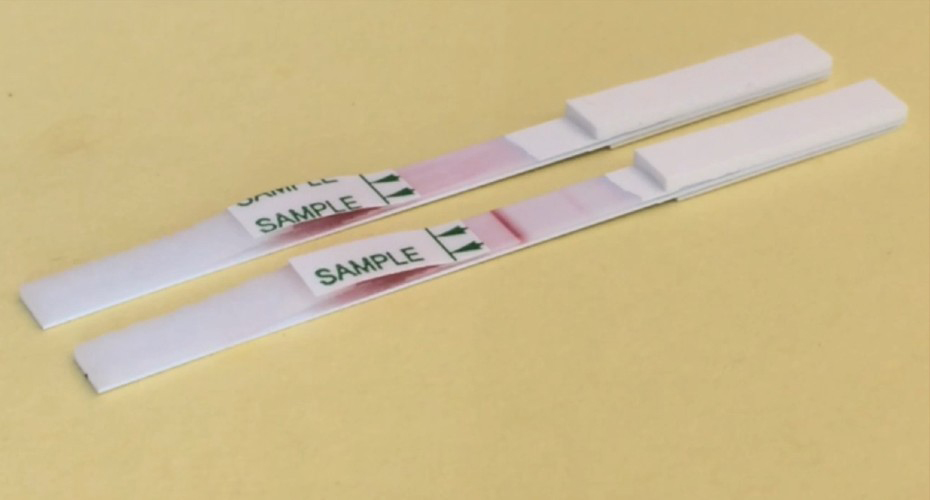
The prototype lateral flow test
A new lateral-flow test could one day save lives across the world through early detection of a deadly fungal disease which dramatically spiked during the COVID-19 pandemic.
The test is being developed for mucormycosis, caused by inhaling the spores of Mucorales fungi, which are ever-present in our environment and harmless for most of us. It is a rare disease, once considered only to affect people with compromised immunity, such as patients undergoing cancer treatment or organ transplants. Before 2019, just over 900,000 cases had been reported globally, mostly in low-and-middle-income countries.
However, COVID-19 caused a worldwide increase in cases of the infection known as rhino-orbital-cerebral mucormycosis (ROCM) or “black fungus disease”, with a particularly dramatic spike in India. This life-threatening and disfiguring disease is most common in people with poorly managed diabetes. This can lead to a combination of high blood sugar (hyperglycaemia) and low blood pH (acidosis), which is found in patients with diabetic ketoacidosis. This impairs immunity to fungal pathogens leaving people far more vulnerable to Mucorales infections.
The second wave of the pandemic created a “perfect storm” of conditions for ROCM to spread rapidly in some regions. The combination of COVID-19 infection, a high background prevalence of diabetes that is poorly managed, and the overuse of corticosteroids to control viral lung inflammation led to a spike of over 40,000 cases of ROCM in a single two-month period in India. The speed of infection and lack of rapid diagnostic tests for the disease resulted in over 3,500 deaths, and severe facial disfigurement in many of the survivors.
Now, Professor Chris Thornton, a scientist at the University of Exeter’s MRC Centre for Medical Mycology has created a novel lateral-flow test which can detect mucormycosis much faster than existing diagnostic techniques. Currently, invasive biopsy samples are cultured in a laboratory, with long turnaround times and poor sensitivity. The new test gives an instant result, using biofluids from the patient. Although still at prototype stage, a new study published in the Journal of Clinical Microbiology, has shown the lateral-flow test to be swift and accurate in identifying the disease.
Professor Thornton, co-author of the study, said: “Mucormycosis is an horrific disease, which spreads rapidly in the body and can leave people horribly facially disfigured, and is often fatal. Early diagnosis is crucial for the best outcome. This study shows that our new test is quick and effective. These exciting results are a critical milestone in the development and validation of the test which we aim to commercialise in the next three years.
The test, which works by a specific antibody binding to a signature molecule secreted by Mucorales fungi to give a positive result, has been developed by Professor Thornton’ s University of Exeter spin-out company ISCA Diagnostics. The company has previously created a highly successful lateral-flow test for another deadly fungal disease, invasive pulmonary aspergillosis, with take-up in hospitals in over 32 countries.
The study was conducted in partnership with colleagues at Besançon University hospital in France. They tested the device in patients with mucormycosis, patients with other fungal infections, and patients without fungal infections. The test detects mucormycosis in 30 minutes with a high level of specificity and sensitivity.
Professor Laurence Millon, Head of Molecular Diagnostics for Invasive Fungal Infections at Besançon University hospital said: “Mucormycosis is incredibly difficult to diagnose requiring lab-based techniques, but the availability of a rapid point-of-care lateral-flow test for the disease will make its detection quicker and cheaper. Its simplicity makes it ideally suited to countries which lack access to diagnostic facilities.”
The new paper is titled ‘Detection of Mucorales antigen in bronchoalveolar lavage samples using a newly developed lateral-flow device’ and is published in the Journal of Clinical Microbiology.